As standard of care, all critically ill patients require routine neurological examination, including pupillary assessment. Assessment of pupil size and the pupillary light reflex (PLR) are critical components of the neurological exam for patients in acute care settings such as the Emergency Department (ED), Intensive Care Unit (ICU), Operating Room (OR), Post Anesthesia Care Unit (PACU), Progressive Care Units (PCU), and diagnostic areas such as Interventional Radiology (IR).(37, 76, 81) Pupillary changes correlate with neurological worsening and yet are often undetectable using traditional manual assessment methods. Manual pupillary assessment, using a flashlight or penlight, is prone to many sources of inaccuracy and is characterized by subjectivity and low interrater reliability.(2, 18, 37, 61, 72, 74, 85, 90)
The Neurological Pupil index™ (NPi®) Pupil Reactivity Assessment Scale
The Neurological Pupil index™ (NPi®) Pupil Reactivity Assessment Scale reflects a comparison of all measured variables in the PLR to known normal observations. On the numeric NPi Scale, an NPi from 3.0 to 4.9 is considered normal, while an NPi less than 3.0 is considered abnormal. (9, 14, 19, 43, 46, 48, 60,66)
NeurOptics® NPi® Pupillometer

The NeurOptics® NPi® Pupillometer is a handheld, automated optical scanner that provides accurate, reliable, and objective measurements of pupillary size, symmetry, and reactivity throughout the entire PLR. The NPi® Scale reflects a comparison of all measured variables in the PLR to a normative model. On the numeric NPi scale, an NPi from 3.0 to 4.9 is considered normal, while an NPi less than 3.0 is considered abnormal.(12, 18, 26, 65, 72, 74, 87, 90)
An abundance of scientific evidence supports NPi as the gold standard in pupillary assessment. The following findings have been objectively demonstrated when quantitative pupillometry and NPi are used:
i. Improvement in interrater reliability of pupillary metrics (2, 69,72, 74)
ii. Accuracy of measurement in common critical care scenarios and medication administration (1, 34, 43, 46, 48, 57, 60, 64, 69, 87, 94)
A recent study of inter-device reliability showed a very high level of agreement between the NPi-200 and NPi-300 pupillometer models among healthy controls and critically ill patients.(93) Although most herein referenced studies are based on the NPi-200, the results are translatable to and remain relevant in demonstrating the benefits of pupillometry and NPi in the NPi-300 Pupillometer.
Pupil Examination Is a Standard of Care and Important to Patient Outcome

The clinical neurological exam is an essential component in the assessment and care of patients with a wide variety of illnesses and injuries.(44, 54, 72) For centuries, clinicians have assessed the pupils of patients with impaired consciousness. Today, clinicians routinely evaluate pupils as part of the neurological exam and monitoring of all critically ill patients, including those with primary neurological injury as well as those at risk of secondary neurologic insults.(5, 37, 54 , 63, 72, 73, 76, 81, 96) Pupillary examination involves assessment of the functional status of two cranial nerves (CN) – the optic nerve (CN II) and the oculomotor nerve (CN III). Cranial nerve dysfunction may signal increased ICP and/or an increased risk of brain herniation.(3, 72)
Pupillary assessment is relied upon to guide decisions regarding patient triage and clinical intervention. Depending on pupillary status, neurosurgeons triage patients into either conservative therapy or surgical evacuation of mass lesions.(72, 76, 85) Patients who undergo prompt intervention such as surgery or hyperosmolar therapy after a new finding of pupil abnormality have a better chance of recovery.(27)
Abnormalities of pupillary response are associated with neurological deterioration and correlate with poor neurological outcomes.(5, 18, 27, 81, 95, 99) Along with other clinical information such as age, mechanism of injury and Glasgow Coma Score (GCS), the PLR is a useful prognostic indicator of survival, functional recovery and long-term outcome.(5, 17, 27, 96)
Manual Pupil Assessment Is Highly Subjective and Inaccurate

Traditionally, pupil assessment has been performed in a subjective manner, using a penlight or flashlight to manually evaluate pupil reactivity and a pupil gauge to estimate pupil size. Common terminology used to describe the PLR and pupil size includes “fixed” or “dilated” as well as “brisk”, “sluggish” or “non-reactive” pupils. These subjective terms are applied without a standardized clinical definition and yield a pronounced level of inter-examiner variability and error.(24, 63, 74)
Manual pupillary assessment is subject to compounded sources of inaccuracies and error and can result in as much as 39% inter-examiner variability.(5, 24, 37, 44, 62, 63, 72, 74) A variety of factors affect the reliability of manual assessment and increase inter-examiner disagreement. These factors may include pinpoint pupils, darkly pigmented irises, examiner skill level and visual acuity, and the strength and orientation of the light stimulus with respect to the patient’s eye.(3, 56) A 2016 study revealed that critical care and neurosurgical nurses consistently underestimated pupil size, were unable to identify anisocoria, and incorrectly assessed pupil reactivity.(44, 65)
The NPi® Pupillometer Is Reliable and Eliminates Subjectivity

The NeurOptics NPi Pupillometer (NeurOptics, Inc., Irvine, CA) is a Class 1 device that is 510k Exempt by the US FDA and CE-marked for the European Economic Area for use in both adults and children. This noninvasive, handheld optical scanner provides reliable and objective measurements of pupillary size, symmetry, and reactivity. The device stimulates pupil constriction with a gentle flash of light as the infrared camera captures 90 images in a 3 second period, measuring 8 different parameters that comprise the entire PLR. A disposable SmartGuard®, programmed with a unique patient identifier, records and stores 168 paired pupil assessments for trending and review throughout the patient’s admission. Launched in July 2021, the latest generation NPi-300 Pupillometer System includes wireless charging capabilities, an incorporated 1D/2D barcode scanner for automated patient identification entry, and other upgraded operational features.
Quantifying pupil reactivity on a numeric scale from 0 to 4.9, the NPi® allows rigorous interpretation and classification of the pupil response. The Pupillometer and the Neurological Pupil index™ (NPi®) Pupil Reactivity Assessment Scale provide objectivity in measurement by comparing the patient’s PLR to normative data in the NPi model. By automatically deriving whether the PLR falls within the normal (“brisk”) range (NPi > 3.0), the abnormal (“sluggish”) range (NPi < 3.0) or is “atypical”, “immeasurable” or “non-reactive” (NPi=0), the NPi Pupillometer provides a reliable and accurate way to quantify and trend pupillary response, offering increased confidence in the neurological assessment. (5, 8, 18, 24, 28, 34, 63, 72, 74)
Numerous studies attest to the reliability of the NPi Pupillometer.(52, 63, 69, 74, 95) In a recent study of unconscious and critically ill cardiac patients, researchers found twice the observer reproducibility and repeatability for quantitative measurements of pupil size with better measurements of reliability, for both size and reactivity, compared to the standard manual assessment. (69)
Monitoring, Treatment and Value in Critical Care
Recognized as an important tool in the ICU, automated pupillometry and NPi are being adopted in hospitals worldwide and becoming accepted as a standard of care for pupillary assessment in patients with a variety of critical illnesses.(3, 81, 85, 105) National and international guidelines now recommend NPi Pupillometry as the preferred method of pupillary assessment. (4, 38, 39, 68, 83)
Neurocritical Care
The NPi Pupillometer provides an objective means of assessing and trending pupillary reactivity across a broad spectrum of neurological conditions including traumatic brain injury (TBI), ischemic and hemorrhagic stroke, cerebral edema, herniation syndrome, and post-operative scenarios.(6, 14, 19, 20, 23, 29, 32, 34, 38, 40, 52, 66)
Quality Improvement
Quality measures help quantify healthcare processes, outcomes, patient perceptions, and organizational structure. They support quality goals for health care, which include effective, safe, efficient, patient-centered, equitable, and timely care. Ongoing quality improvement is a cornerstone for all hospitals and automated pupillometry is a natural fit as hospital quality systems continue to evolve.
Improved Quality of Neurological Exam
Assessment of pupil size and reactivity is a fundamental aspect of the neurological examination. However, manual pupil assessments (using a penlight or flashlight) are subjective and fraught with a high degree of inter-examiner variability. In a 2015 study, two examiners under identical conditions evaluated the pupils of consented patients. Over 2300 paired assessments were performed, followed by assessment with the pupillometer. The study showed only moderate inter-rater reliability between practitioners for pupil size, shape and reactivity. A major finding was that practitioners agreed less than half the time about non-reactive pupils, and more than 66% of the pupils scored as non-reactive by practitioners were actually reactive when measured by NPi Pupillometry.(74) Disagreement about non-reactive pupils can have significant consequences for the patient. This study and others support the use of automated pupillometry to improve the reliability and objectivity of pupillary assessment.
A quality improvement project, published by The University of Pittsburgh Medical Center, looked at adoption of the Pupillometer for routine care in a Neurotrauma ICU. This center reported that the Pupillometer led to increased confidence in the neurological examination, enhanced clinical decision making, and added value to patient care.(5)
Automated pupillometry provides completely accurate, reliable, and objective pupil data, independent of examiner, resulting in quality improvement for this important component of the neurological examination.
Adherence to Hospital Protocols/Reduction in Manual Entry Errors
Standard hospital protocols and guidelines for neurologically injured patients call for pupil assessments at regularly scheduled intervals. A typical nursing day with a critically ill patient requires coordination of care, diagnostic testing, frequent assessment and monitoring, medication administration, supporting the patient’s family, and many other complex and time-sensitive tasks. To save time and reduce errors often associated with manual data entry, patient data on the SmartGuard can be uploaded to the electronic medical record (EMR) system through coordination with your information technology (IT) and informatics teams. The pupillometer date and time stamp allow data review and trending from the time of admission throughout the patient’s hospital course, providing additional means to monitor compliance with protocols, guidelines, and quality initiatives.
Staffing: Cost and Time Savings
Automated pupillometry has been shown to decrease nursing workload associated with frequent pupillary assessment. To save valuable nursing time and resources, The University of Texas Southwestern Medical Center has successfully instituted a practice change in the Neuroscience ICU in which patient care technicians (unlicensed assistive personnel) obtain routine pupillometer measurements on designated patients. Results are reported to the assigned RN for interpretation and assessment of patient status.(92) In accordance with the state Board of Nursing and Nursing Practice Act, pupillometry measurements may be delegated to unlicensed assistive personnel with appropriate education.(92)
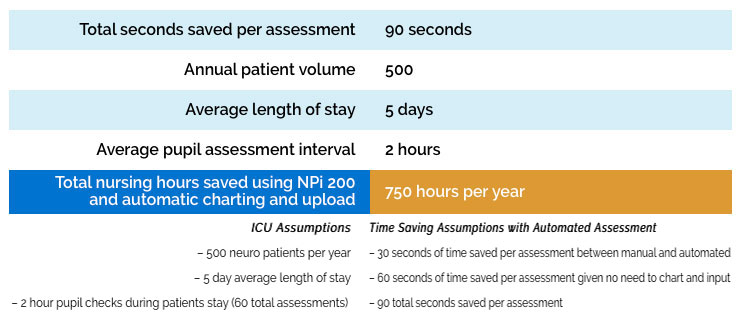
One study, illustrated below, showed that nurses saved on average 19.8 min per patient per day using automated pupillometry with direct data upload to the patient EMR.(102) Time saved by use of automated pupillometry increases with increasing frequency of serial pupillary examinations. This suggests that improvement in workforce efficiency by using automated pupillometers may translate into increased productivity and, ultimately, cost-saving benefits.(81, 92) As nursing leadership looks to improve efficiency in workflow and staffing, NPi Pupillometers at each bedside can assist in that effort.
Manual Pupil Assessment Technique
Manual pupil assessments (penlight) are subjective and fraught with a high degree of inter-examiner variability. It is well documented that automated pupillary assessment solves these problems, but manual pupil assessment can also take more time than automated pupillometry and little has been discussed about this.
A paired assessment with the pupillometer takes a clinician about 15 seconds. Manual pupil assessment can be confounded by several issues: Visual acuity of the examiner, dark eyes or small pupils of the patient, ambient light conditions and the subjectivity and skill/experience level of the examiner. As a result, in some patients, a clinician will often pass the penlight multiple times to try and confirm what he/she sees and a manual assessment can take even more time. In other cases, if the clinician is not sure, or if there is a suspected pupil change, another opinion might be sought. This involves an additional person and several minutes more of time. As a single measurement, these differences might not seem meaningful but given the frequency of pupil exams, these differences are significant over time.
Charting and Inputting Data
Some clinicians will complete the exam and immediately record the pupil measurement data into the terminal, while others will complete the pupil exam, continue with necessary patient care, and then later go to the terminal, log in, input the data and log out. Nurses at a high volume neuro ICU were recently timed and, on average, these charting and data entry steps took about one minute. Automatic data upload will eliminate the need to manually chart and input data.
Annual Cost Savings Example
Building an Effective Pupillometry Program
To achieve the benefits previously identified, successful adoption of pupillometry relies upon collaboration of a multidisciplinary team including nurses, providers, nursing leadership, biomedical engineering, IT, and supply chain management. Additionally, there are three key components to building an effective pupillometry program – eliminating barriers, establishing protocols and education.
Eliminating Barriers
Anticipating and eliminating barriers promotes successful adoption of new technology. Ensuring an appropriate number of and easy access to NPi Pupillometers based on unit size/layout is essential for optimizing nursing workflow and routine. Many hospitals dedicate one pupillometer to each patient room or one to every other room. A recent study showed that allocation of one pupillometer per patient room significantly improved compliance with pupillary assessment among nurses in the Neuro ICU.(89) A standardized process for ordering and stocking SmartGuards is equally important to ensure uninterrupted availability for patient care.
Another consideration is planning for documentation, including which values will be documented (typically pupil size and NPi) and in what format – paper flowsheet, fields added for manual EMR entry, or automatic upload. Examining their five-year experience with pupillometry and the ability to interface with the EMR, nurses across 6 different patient care units at University of California Irvine Health found that directly uploading pupillometer data to the EMR improved nursing workflow and improved documentation of pupillary findings and changes.(97) More information on EMR integration can be found at https://neuroptics.com/emr-integration/
Establishing Protocols
Much of the care provided to critically ill patients is driven by protocols based on evidence and best-practice guidelines. To standardize use and provide the most benefit to patients and clinicians, it is important to establish unit protocols and guidelines for use of the NPi Pupillometer. Essential components of a comprehensive protocol include 1) clear indications for use, including both primary neurological injuries as well as secondary indications (CA, ARDS, AMS etc); 2) a focus on baseline assessment at the time of admission and trending of values from subsequent exams; 3) procedural steps for use; and 4) guidelines for documentation and reporting abnormal values. Sample protocols are available from your NeurOptics representative for use when developing protocols or guidelines in your institution.
Education
Nursing and provider education are essential to the success of Pupillometer integration into clinical practice. NeurOptics stands ready to support education with local sales representatives and a network of RN Clinical Specialists. Together with clinical educators/managers and key personnel, NeurOptics works to develop a comprehensive day/night/weekend education plan according to institutional requirements. While on-site education is preferred, virtual education in a variety of formats can also be provided.
Initial education, at the time of pupillometer installation/rollout, focuses on operation of the NPi Pupillometer and conceptual understanding of its clinical use and benefits. Follow up education, scheduled four to six weeks later and periodically as needed, aims to reinforce operational skills and integration of pupillometry into routine clinical practice. Our education team is also available to support annual skills/competency days, Grand Rounds and other formal presentations.
NeurOptics provides and promotes many educational resources on the website (www.NeurOptics.com), including product information, instructional videos, webinar recordings, and clinical publications.
Appendix
Fig. 1 The NPi®-300 Pupillometer System with Wireless Charging Station and Incorporated Barcode Scanner

Please contact your local representative for more information on the features and availability of the NPi®-300 Pupillometer.
Fig. 2 Baseline and Trending with the Neurological Pupil index™ (NPi®) Pupil Reactivity Assessment Scale
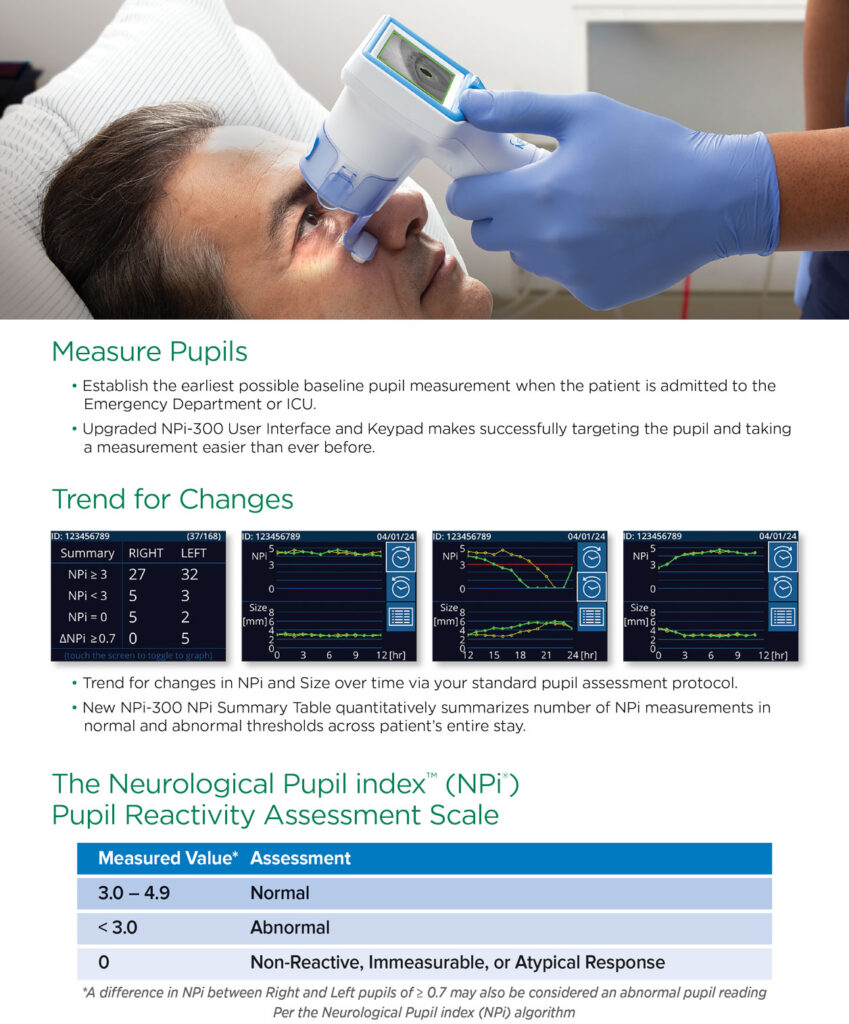
Fig. 3 Clinical Reference Texts and Guidelines Including Pupillometry and NPi
3a.
3b.
3c.
3a. American Association of Critical-Care Nurses. AACN Procedure Manual for Progressive and Critical Care. 8th edition. Johnson ed. Elsevier;2023:866-870.(10)
3b. American Association of Neuroscience Nurses. AANN Core Curriculum for Neuroscience Nursing. 7th edition. Littlejohns, McNett, Olson eds. AANN;2022:167-168.(12)
3c. Hickey JV, Strayer A. The Clinical Practice of Neurological and Neurosurgical Nursing. 8th edition. Wolters Kluwer; 2020:168-170.(37)

Bibliography
Bibliography
1. Achamallah N, Fried J, Love R, Matusov Y, Sharma R. Pupillary light reflex is not abolished by epinephrine and atropine given during advanced cardiac life support in patients who achieve return of spontaneous circulation. J Intensive Care Med. Apr 2021;36(4):459-465. doi:10.1177/0885066620906802
2. Al-Obaidi SZ, Atem FD, Stutzman SE, Olson DM. Impact of increased intracranial pressure on pupillometry: A replication study. Crit Care Explor. Oct 2019;1 (10): e0054. doi:10.1097/CCE.0000000000000054
3. Al-Obaidi S, Atem F, Stutzman SE, Aiyagari V, Olson DM. Investigating the association between eye colour and the Neurological Pupil index. Aust Crit Care. Sep 2020;33(5):436-440. doi:10.1016/j.aucc.2019.10.001
4. American Heart Association. Highlights of the 2020 American Heart Association Guidelines for CPR and ECC. 2020. https://cpr.heart.org/-/media/cpr-files/cpr-guidelines-files/highlights/hghlghts_2020_ecc_guidelines_english.pdf
5. Anderson M, Elmer J, Shutter L, Puccio A, Alexander S. Integrating quantitative pupillometry into regular care in a neurotrauma intensive care unit. J Neurosci Nurs. Feb 2018;50(1):30-36. doi:10.1097/JNN.0000000000000333
6. Aoun SG, Stutzman SE, Vo PN, et al. Detection of delayed cerebral ischemia using objective pupillometry in patients with aneurysmal subarachnoid hemorrhage. J Neurosurg. Jan 2019; 132(1):27-32. doi:10.3171/2018.9.JNS181928
7. Aoun SG, Welch BG, Cortes M, et al. Objective pupillometry as an adjunct to prediction and assessment for oculomotor nerve injury and recovery: Potential for practical applications. World Neurosurg. Jan 2019;121:e475-e480. doi:10.1016/j.wneu.2018.09.140
8. Bader MK. Gizmos and gadgets for the neuroscience intensive care unit. J Neurosci Nurs. Aug 2006;38(4):248-60. doi:10.1097/01376517-200608000-00008
9. Battley J, Marshall J, Olson DW, Stutzman S, Reyes R. Quantitative pupillometry is not impacted by IV opioid or sedative bolus dosing. Presented at: 2023 American Academy of Neurology (AAN) Annual Meeting. April 2023. https://neuroptics.com/portfolio_page/quantitative-pupillometry-is-not-impacted-by-iv-opioid-or-sedative-bolus-dosing/
10. Bazil JC. Pupillometry. In Johnson K, ed. AACN Procedure Manual for Progressive and Critical Care. 8th edition. Elsevier;2023:866-870:chap 90.
11. Behrends M, Niemann CU, Larson MD. Infrared pupillometry to detect the light reflex during cardiopulmonary resuscitation: A case series. Resuscitation. Oct 2012;83(10):1223-8. doi:10.1016/j.resuscitation.2012.05.013
12. Berlin T, Lang C, Puccio A. Technology. In: Littlejohns L, McNett M, Olson D, eds. AANN Core Curriculum for Neuroscience Nursing. 7th ed. American Association of Neuroscience Nurses; 2022:167-168:chap 7.
13. Boev AN, Fountas KN, Karampelas I, et al. Quantitative pupillometry: Normative data in healthy pediatric volunteers. J Neurosurg. Dec 2005;103(6 Suppl):496-500. doi:10.3171/ped.2005.103.6.0496
14. Bower MM, Sweidan AJ, Xu JC, Stern-Nezer S, Yu W, Groysman LI. Quantitative pupillometry in the intensive care unit. J Intensive Care Med. Oct 2019. doi:10.1177/0885066619881124
15. Breckwoldt J, Arntz HR. Infrared pupillometry during cardiopulmonary resuscitation for prognostication: A new tool on the horizon? Resuscitation. Oct 2012;83(10):1181-2. doi:10.1016/j.resuscitation.2012.06.020
16. Brown JT, Connelly M, Nickols C, Neville KA. Developmental changes of normal pupil size and reactivity in children. J Pediatr Ophthal Strabismus. May-Jun 2015;52(3):147-51. doi:10.3928/01913913-20150317-11
17. Butt AA, Aten FD, Stutzman SE, Aiyagari V, Venkatachalam AM, Olson DM, Yokobori S. Contribution of pupillary light reflex assessment to Glasgow Coma Scale for prognostication in patients with traumatic brain injury. J NeurocritCare. 2021;14(1):29-35. doi:10.18700/jnc.210001
18. Chen JW, Gombart ZJ, Rogers S, Gardiner SK, Cecil S, Bullock RM. Pupillary reactivity as an early indicator of increased intracranial pressure: The introduction of the Neurological Pupil index. Surg Neurol Int. 2011;2:82. doi:10.4103/2152-7806.82248
19. Chen JW, Vakil-Gilani K, Williamson KL, Cecil S. Infrared pupillometry, the Neurological Pupil index and unilateral pupillary dilation after traumatic brain injury: Implications for treatment paradigms. Springerplus. 2014;3:548. doi:10.1186/2193-1801-3-548
20. Cortes MX, Siaron KB, Nadim HT, Ahmed KM, Romito JW. Neurological Pupil Index as an indicator of irreversible cerebral edema: A cases. J Neurosci Nurs. Jun 2021;53(3):145-148. doi:10.1097/JNN.0000000000000584
21. Crippa IA, Pelosi P, Quispe-Cornejo AA, et al. Automated pupillometry as an assessment tool for intracranial hemodynamics in septic patients. Cells. Jul 2022;11(14). doi:10.3390/cells11142206
22. Douglas VC, Josephson SA. Altered mental status. Continuum (Minneap Minn). Oct 2011; 17(5):967-83. doi:10.1212/01.CON.0000407055.17661.33
23. Dowlati E, Sarpong K, Kamande S, et al. Abnormal neurological pupil index is associated with malignant cerebral edema after mechanical thrombectomy in large vessel occlusion patients. Neurol Sci. Dec 2021;42(12):5139-5148. doi:10.1007/s10072-021-05218-x
24. Du R, Meeker M, Bacchetti P, Larson MD, Holland MC, Manley GT. Evaluation of the portable infrared pupillometer. Neurosurgery. Jul 2005;57(1):198-203. doi:10.1227/01.neu.0000163425.79170.cb
25. Dundaroz R, Turkbay T, Erdem U, Congologlu A, Sakallioglu O, Tascilar E. Pupillometric assessment of autonomic nervous system in children with functional enuresis. Int UrolNephrol. 2009;41(2):231-5. doi:10.1007/s11255-008-9481-1
26. El Ahmadieh TY, Bedros NM, Stutzman SE, et al. Automated pupillometry as a triage and assessment tool in patients with traumatic brain injury. World Neurosurg. Oct 2020; doi:10.1016/j.wneu.2020.09.152
27. Emelifeonwu JA, Reid K, Rhodes JK, Myles L. Saved by the pupillometer! – A role for pupillometry in the acute assessment of patients with traumatic brain injuries? Brain Inj. 2018;32(5):675-677. doi:10.1080/02699052.2018.1429021
28. Fountas KN, Kapsalaki EZ, Machinis TG, Boev AN, Robinson JS, Troup EC. Clinical implications of quantitative infrared pupillometry in neurosurgical patients. NeurocritCare. 2006;5(1):55-60. doi:10.1385/NCC:5:1:55
29. Freeman AD, McCracken CE, Stockwell JA. Automated pupillary measurements inversely correlate with increased intracranial pressure in pediatric patients with acute brain injury or encephalopathy. Pediatr CritCare Med. Aug 2020;21(8):753-759. doi:10.1097/PCC.0000000000002327
30. Freeman WD, Barrett KM, Vatz KA, Demaerschalk BM. Future neurohospitalist: teleneurohospitalist. Neurohospitalist. Oct 2012;2(4):132-43. doi:10.1177/1941874412450714
31. Ghauri MS, Ueno A, Mohammed S, Miulli DE, Siddiqi J. Evaluating the reliability of neurological pupillary index as a prognostic measurement of neurological function in critical care patients. Cureus. Sep 2022;14(9):e28901. doi:10.7759/cureus.28901
32. Giamarino K, Blessing R, Boelter C, Thompson JA, Reynolds SS. Exploring the relationship between objective pupillometry metrics and midline shift. J Neurosci Nurs. Dec 2021;53(6):233-237. doi:10.1097/JNN.0000000000000614
33. Godau J, Bharad K, Rösche J, et al. Automated pupillometry for assessment of treatment success in nonconvulsive status epilepticus. Neurocrit Care. Jul 2021. doi:10.1007/s12028-021-01273-6
34. Godau J, Bierwirth C, Rösche J, Bösel J. Quantitative infrared pupillometry in nonconvulsive status epilepticus. Neurocrit Care. Nov 2020. doi:10.1007/s12028-020—1149-124.
35. Han JH, Wilber ST. Altered mental status in older patients in the emergency department. Clin Geriatr Med. Feb 2013;29(1):101-36. doi:10.1016/j.cger.2012.09.005
36. Hatcher-Martin JM, Adams JL, Anderson ER, et al. Telemedicine in neurology: Telemedicine Work Group of the American Academy of Neurology update. Neurology. Jan 2020;94(1):30-38. doi:10.1212/WNL.0000000000008708
37. Hickey JV, Strayer A. The Clinical Practice of Neurological and Neurosurgical Nursing. Eighth edition. ed. Wolters Kluwer; 2020:168-170.
38. Hill M, Moreda M, Navarro J, Mulkey M. Assessing patients with altered level of consciousness. Crit Care Nurse. 2023;43(4):58-65. doi:10.4037/ccn2023449
39. Hirsch KG, Abella BS, Amorim E, Bader MK, Barletta JF, Berg K, et al. Critical care management of patients after cardiac arrest: A scientific statement from the American Heart Association and Neurocritical Care Society. Neurocritical Care. Published online Dec 1, 2023. doi.org/10.1007/s12028-023-01871-6
40. Hupp C, Cronin M, Kim ISY, Ong C. Quantitative pupillometry in patients with surgical decompression. 2023 American Academy of Neurology (AAN) Annual Meeting. April 2023. https://neuroptics.com/portfolio_page/quantitative-pupillometry-in-patients-with-surgical-decompression/
41. Jahns FP, Miroz JP, Messerer M, et al. Quantitative pupillometry for the monitoring of intracranial hypertension in patients with severe traumatic brain injury. Crit Care. May 2019;23(1):155. doi:10.1186/s13054-019-2436-3
42. Jiang J, Goldman R, Huff E, Hanna A, Bhalala U: Neurological Pupil index (NPi) monitoring using pupillometer and outcomes in critically ill children. 2023 Society of Critical Care Medicine (SCCM) 52nd Critical Care Congress. January 2023. https://neuroptics.com/portfolio_page/neurological-pupil-index-npi-monitoring-using-pupillometer-and-outcomes-in-critically-ill-children/
43. Jolkovsky EL, Fernandez-Penny FE, Alexis M, Benson LN, Wang BH, Abella BS. Impact of acute intoxication on quantitative pupillometry assessment in the emergency department. J Am Coll Emerg Physicians Open. Oct 2022;3(5):e12825. doi:10.1002/emp2.12825
44. Kerr RG, Bacon AM, Baker LL, et al. Underestimation of pupil size by critical care and neurosurgical nurses. Am J Crit Care. May 2016;25(3):213-9. doi:10.4037/ajcc2016554
45. Kim TJ, Ko SB. Implication of Neurological Pupil Index for monitoring of brain edema. Acute Crit Care. Feb 2018;33(1):57-60. doi:10.4266/acc.2017.00213
46. Kim TJ, Park SH, Jeong HB, et al. Neurological Pupil index as an indicator of neurological worsening in large hemispheric strokes. Neurocrit Care. Oct 2020;33(2):575-581. doi:10.1007/s12028-020-00936-0
47. Kim DW, Jo YH, Park SM, Lee DK, Jang DH. Neurological pupil index during cardiopulmonary resuscitation is associated with admission to ICU in non-traumatic out-of-hospital cardiac arrest patients. Signa Vitae. 2023. doi:10.22514/sv.2022.038.
48. Larson MD. Mechanism of opioid-induced pupillary effects. Clin Neurophysiol. Jun 2008;119(6): 1358-64. doi:10.1016/j.clinph.2008.01.106
49. Lee H, Choi SH, Park B, Hong YH, Lee HB, Jeon SB. Quantitative assessments of pupillary light reflexes in hospital-onset unresponsiveness. BMC Neurol. Jun 2021;21(1):234. doi:10.1186/s12883-021-02275-9
50. Lee S, Jung DE, Park D, et al. Intraoperative neurological pupil index and postoperative delirium and neurologic adverse events after cardiac surgery: an observational study. Sci Rep. Aug 2023;13(1):13838. doi:10.1038/s41598-023-41151-z
51. Lele AV, Wahlster S, Khadka S, et al. Neurological Pupillary index and disposition at hospital discharge following ICU admission for acute brain injury. J Clin Med. Jun 2023;12(11):3806. doi:10.3390/jcm12113806
52. Lussier BL, Olson DM, Aiyagari V. Automated pupillometry in neurocritical care: Research and practice. Curr Neurol Neurosci Rep. Aug 2019;19(10):71. doi:10.1007/s11910-019-0994-z
53. Lussier BL, Stutzman SE, Atem F, et al. Distributions and reference ranges for automated pupillometer values in neurocritical care patients. J Neurosci Nurs. Dec 2019;51(6):335-340. doi:10.1097/JNN.0000000000000478
54. Manley GT, Larson MD. Infrared pupillometry during uncal herniation. J Neurosurg Anesthesiol. Jul 2002;14(3):223-8. doi:10.1097/00008506-200207000-00009
55. Marshall M, Deo R, Childs C, Ali A. Feasibility and variability of automated pupillometry among stroke patients and healthy participants: potential implications for clinical practice. J Neurosci Nurs. Apr 2019;51(2):84-88. doi:10.1097/JNN.0000000000000416
56. Martínez-Ricarte F, Castro A, Poca MA, et al. Infrared pupillometry: Basic principles and their application in the non-invasive monitoring of neurocritical patients. Neurologia. Jan-Feb 2013;28(1):41-51. doi:10.1016/j.nrl.2010.07.028
57. Matousková O, Slanar O, Chytil L, Perlík F. Infrared pupilometry as a biomarker of drug effects. Cas Lek Cesk. 2010;149(2):66-8.
58. Mazhar K, Olson DM, Atem FD, et al. Supratentorial intracerebral hemorrhage volume and other CT variables predict the neurological pupil index. Clin Neurol Neurosurg. Jan 2021;200:106410. doi:10.1016/j.clineuro.2020.106410
59. McGetrick ME, Schneider N, Olson DM, Aiyagari V, Miles D. Automated infrared pupillometer use in assessing the neurological status in pediatric neurocritical care patients: Case reports and literature review; J Child Science 2021;11(01):e125-e132. doi: 10.1055/s-0041-1731074
60. McKay RE, Larson MD. Detection of opioid effect with pupillometry. Auton Neurosci. Nov 2021; 235:102869. doi:10.1016/j.autneu.2021.102869
61. McNett M, Moran C, Grimm D, Gianakis A. Pupillometry trends in the setting of increased intracranial pressure. J Neurosci Nurs. Dec 2018;50(6):357-361. doi:10.1097/JNN.0000000000000401
62. McNett M, Moran C, Janki C, Gianakis A. Correlations between hourly pupillometer readings and intracranial pressure values. J Neurosci Nurs. Aug 2017;49(4):229-234. doi:10.1097/JNN.0000000000000290
63. Meeker M, Du R, Bacchetti P, et al. Pupil examination: Validity and clinical utility of an automated pupillometer. J Neurosci Nurs. Feb 2005;37(1):34-40.
64. Miroz JP, Ben-Hamouda N, Bernini A, et al. Neurological Pupil index for early prognostication after venoarterial extracorporeal membrane oxygenation. Chest. May 2020;157(5):1167-1174. doi:10.1016/j.chest.2019.11.037
65. Morelli P, Oddo M, Ben-Hamouda N. Role of automated pupillometry in critically ill patients. Minerva Anestesiol. Sep 2019;85(9):995-1002. doi:10.23736/S0375-9393.19.13437-2
66. Natzeder S, Mack DJ, Maissen G, Strässle C, Keller E, Muroi C. Portable infrared pupillometer in patients with subarachnoid hemorrhage: Prognostic value and circadian rhythm of the Neurological Pupil index (NPi). J Neurosurg Anesthesiol. Oct 2019;31(4):428-433. doi:10.1097/ANA.0000000000000553
67. Neerukonda SV, Schneider NJ, Aiyagari V, Olson DM. Automated pupillometry value differences serve as a prognostic indicator even when they are within normal range. The Journal of Neurological and Neurosurgical Nursing. Dec 2021;10(4):168–174. doi:10.15225/PNN.2021.10.4.5
68. Nolan JP, Sandroni C, Böttiger BW, et al. European Resuscitation Council and European Society of Intensive Care Medicine Guidelines 2021: Post-resuscitation care. Resuscitation. Apr 2021;161:220-269. doi:10.1016/j.resuscitation.2021.02.012
69. Nyholm B, Obling L, Hassager C, et al. Superior reproducibility and repeatability in automated quantitative pupillometry compared to standard manual assessment, and quantitative pupillary response parameters present high reliability in critically ill cardiac patients. PLoS One. 2022;17(7):e0272303. doi:10.1371/journal.pone.0272303
70. Oddo M, Sandroni C, Citerio G, et al. Quantitative versus standard pupillary light reflex for early prognostication in comatose cardiac arrest patients: An international prospective multicenter double-blinded study. Intensive Care Med. Dec 2018;44(12):2102-2111. doi:10.1007/s00134-018-5448-6
71. Oddo M, Taccone FS, Petrosino M, Badenes R, Blandino-Ortiz A, Bouzat P, Caricato A, et al.: The Neurological Pupil index for outcome prognostication in people with acute brain injury (ORANGE): A prospective, observational, multicentre cohort study. The Lancet Neurology. August 28, 2023. doi.org/10.1016/S1474-4422(23)00271-5.
72. Olson DM, Fishel M. The use of automated pupillometry in critical care. Crit CareNurs Clin North Am. Mar 2016;28(1):101-7. doi:10.1016/j.cnc.2015.09.003
73. Olson DM, Stutzman SE, Atem F, et al. Establishing normative data for pupillometer assessment in neuroscience intensive care: The “END-PANIC” Registry. J Neurosci Nurs. Aug 2017;49(4):251-254. doi:10.1097/JNN.0000000000000296
74. Olson DM, Stutzman S, Saju C, Wilson M, Zhao W, Aiyagari V. Interrater reliability of pupillary assessments. Neurocrit Care. Apr 2016;24(2):251-7. doi:10.1007/s12028-015-0182-1
75. Ong C, Hutch M, Barra M, Kim A, Zafar S, Smirnakis S. Effects of osmotic therapy on pupil reactivity: Quantification using pupillometry in critically ill neurologic patients. Neurocrit Care. April 2019;30(2):307-315. doi:10.1007/s12028-018-0620-y
76. Ong C, Hutch M, Smirnakis S. The effect of ambient light conditions on quantitative pupillometry. Neurocrit Care. April 2019;30(2):316-321. doi:10.1007/s12028-018-0607-8
77. Osman M, Stutzman SE, Atem F, et al. Correlation of objective pupillometry to midline shift in acute stroke patients. J Stroke Cerebrovasc Dis. Jul 2019;28(7):1902-1910. doi:10.1016/j.jstrokecerebrovasdis.2019.03.055
78. Papangelou A, Zink EK, Chang WW, et al. Automated pupillometry and detection of clinical transtentorial brain herniation: A case series. Mil Med. Jan 2018;183(1-2):e113-e121. doi:10.1093/milmed/usx018
79. Patwari PP, Stewart TM, Rand CM, et al. Pupillometry in congenital central hypoventilation syndrome (CCHS): Quantitative evidence of autonomic nervous system dysregulation. Pediatr Res. Mar 2012;71(3):280-5. doi:10.1038/pr.2011.38
80. Payen JF, Isnardon S, Lavolaine J, Bouzat P, Vinclair M, Francony G. Pupillometry in anesthesia and critical care. Ann Fr Anesth Reanim. Jun 2012;31(6):e155-159. doi:10.1016/j.annfar.2012.04.020
81. Phillips SS, Mueller CM, Nogueira RG, Khalifa YM. A systematic review assessing the current state of automated pupillometry in the NeuroICU. Neurocrit Care. Aug 2019;31(1):142-161. doi:10.1007/s12028-018-0645-2
82. Privitera CM, Neerukonda SV, Aiyagari V, et al. A differential of the left eye and right eye neurological pupil index is associated with discharge modified Rankin scores in neurologically injured patients. BMC Neurol. Jul 2022;22(1):273. doi:10.1186/s12883-022-02801-3
83. Rajajee V, Muehlschlegel S, Wartenberg KE,et al. Guidelines for Neuroprognostication in Comatose Adult Survivors of Cardiac Arrest. Neurocritical Care. 2023 Jun;38(3):533-563. doi: 10.1007/s12028-023-01688-3.
84. Rana C, Moreno J, Marshall J, Olson DM, Aiyagari V: Neuroradiological correlates of abnormal pupillary light reflex findings in patients in the Neuroscience Intensive Care Unit (NSICU). 2023 Neurocritical Care Society (NCS) 21st Annual Meeting – August 2023. https://neuroptics.com/portfolio_page/neuroradiological-correlates-of-abnormal-pupillary-light-reflex-findings-in-patients-in-the-neuroscience-intensive-care-unit-nsicu/
85. Rasulo FA, Togni T, Romagnoli S. Essential noninvasive multimodality neuromonitoring for the critically ill patient. Crit Care. Mar 2020;24(1):100. doi:10.1186/s13054-020-2781-2
86. Riker RR, Sawyer ME, Fischman VG, et al. Neurological Pupil index and pupillary light reflex by pupillometry predict outcome early after cardiac arrest. Neurocrit Care. Feb 2020;32(1):152-161. doi:10.1007/s12028-019-00717-4
87. Rollins MD, Feiner JR, Lee JM, Shah S, Larson M. Pupillary effects of high-dose opioid quantified with infrared pupillometry. Anesthesiology. Nov 2014;121(5):1037-44. doi:10.1097/ALN.0000000000000384
88. Romagnosi F, Bernini A, Bongiovanni F, et al. Neurological Pupil index for the early prediction of outcome in severe acute brain injury patients. Brain Sciences. May 2022;12(5). doi:10.3390/brainsci12050609
89. Saju C, Ortega S, Hill M, Barnes A, Stutzman S. Does increased access impact compliance of pupillometer assessments? Presented at: 2nd Annual International Neuroscience Nursing Research Symposium (INNRS). Aug 2018. https://neuroptics.com/portfolio_page/does-increased-access-impact-compliance-of-pupillometer-assessments/
90. Shoyombo I, Aiyagari V, Stutzman SE, et al. Understanding the relationship between the Neurologic Pupil index and constriction velocity values. Sci Rep. May 2018;8(1):6992. doi:10.1038/s41598-018-25477-7
91. Smith AT, Han JH. Altered mental status in the emergency department. SeminNeurol. Feb 2019; 39(1):5-19. doi:10.1055/s-0038-1677035
92. Stout D, Dullaway J, McMahan H, Daniel BA, Olson DM. Reflections on patient care technicians obtaining pupillometer readings in a neuroscience intensive care unit. J Neurosci Nurs. Dec 2022; 54(6):245-246. doi:10.1097/JNN.0000000000000676
93. Stutzman S, Iype P, Marshall J, et al. Inter-device reliability of the NPi-200 and NPi-300 pupillometers. J Clin Neurosci. Jun 2022;100:180-183. doi:10.1016/j.jocn.2022.04.023
94. Stutzman S, Olson DM, Venkatachalam AM, Barnes A, Atem FD. The presence of cataract does not influence assessment of the pupillary light reflex using automated pupillometry. Journal of Health and Caring Sciences. Dec 2021;3(2):85-95. doi:10.37719/jhcs.2021.v3i2.oa001
95. Taylor WR, Chen JW, Meltzer H, et al. Quantitative pupillometry, a new technology: Normative data and preliminary observations in patients with acute head injury. Technicalnote. J Neurosurg. Jan 2003;98(1):205-13. doi:10.3171/jns.2003.98.1.0205
96. Tokuda Y, Nakazato N, Stein GH. Pupillary evaluation for differential diagnosis of coma. Postgrad Med J. Jan 2003;79(927):49-51. doi:10.1136/pmj.79.927.49
97. Tran DK. Five-year experience with an automated pupillometer system: Implementation and nursing attitudes. Presented at: 2021 Society of Critical Care Medicine (SCCM) 50th Critical Care Congress. February 2021. https://neuroptics.com/portfolio_page/five-year-experience-with-an-automated-pupillometer-system-implementation-and-nursing-attitudes/
98. Trent T, Vashisht A, Novakovic S, et al. Pupillary light reflex measured with quantitative pupillometry has low sensitivity and high specificity for predicting neuroworsening after traumatic brain injury. J Am Assoc Nurse Pract. Feb 2023;35(2):130-134. doi:10.1097/JXX.0000000000000822
99. Veerapaneni D, Daneshmand A, Kim SY, Nguyen C, Greer D, Ong C: Prognostic pupil reactivity markers within the first 72 hours of traumatic brain injury. 2023 Neurocritical Care Society (NCS) 21st Annual Meeting – August 2023. https://neuroptics.com/portfolio_page/prognostic-pupil-reactivity-markers-within-the-first-72-hours-of-traumatic-brain-injury/
100. Wainwright M. Pediatric neurological assessment and monitoring. In: Fuhrman B, Zimmerman J, eds. Pediatric Critical Care. 4th ed. St. Louis, MO: Mosby; 2011:746-758:chap 55.
101. Wechsler LR. The teleneurology revolution. Ann Neurol. Oct 2020;88(4):656-657. doi:10.1002/ana.25849
102. Wilkie, AC: Nursing time savings study: Pupillary assessment times. Poster presentation. Irvine, CA: NeuroSurgical ICU, University of California Irvine Medical Center; 2015. https://neuroptics.com/wp-content/uploads/2017/02/Wilkie-A.-Pupillar-Assessment-Poster-Pres.-2015.pdf
103. WHO-ICRC. Basic Emergency Care: approach to the acutely ill and injured. Oct 2018; Available for download online: https://www.icrc.org/en/publication/basic-emergency-care-approach-acutely-ill-and-injured
104. Xiao HY, Wang YX, Xu TD, et al. Evaluation and treatment of altered mental status patients in the emergency department: Life in the fast lane. World J Emerg Med. 2012;3(4):270-7. doi:10.5847/wjem.j.issn.1920-8642.2012.04.006
105. Zafar SF, Suarez JI. Automated pupillometer for monitoring the critically ill patient: A critical appraisal. J Crit Care. Aug 2014;29(4):599-603. doi:10.1016/j.jcrc.2014.01.012



